Issue 4: Brain, Hormones & the Big O
Understanding the Neurochemical Symphony of Sexual Response
I. Introduction: More Than Just Physical
After writing about orgasm recognition, I kept getting the same question: "But what's actually happening in my brain?"
It's a question that fascinated me too. Understanding the electrical system of your body is one thing, but the neurochemical cascade that creates the euphoria, the bonding, the sometimes overwhelming emotional responses - that's where things get really interesting.
When I started digging into the research on what happens in your brain during sexual response, I realized how much the neurochemical aspect explains about my own experiences.
👉 Why do I sometimes feel like crying after an intense orgasm?
👉 Why does good sex help reset my anxiety better than any meditation app?
👉 Why do I feel so connected to my partner afterward, even when we started out feeling distant?
The answers lie in a sophisticated chemical orchestra playing out in your brain - a precise sequence of neurotransmitters and hormones that creates not just physical pleasure, but emotional bonding, stress relief, and even spiritual-like experiences.
Understanding this neurochemical symphony doesn't just satisfy curiosity; it helps explain why sexual wellness affects your entire well-being.
This isn't about turning sex into a science experiment. It's about appreciating the remarkable complexity of what your brain accomplishes during sexual response, and why taking care of your sexual health is actually taking care of your mental and emotional health too.
Individual Variations: Why Your Brain is Unique
The neurochemical symphony plays differently for everyone. ADHD brains might need different strategies to quiet analytical thinking, while autistic individuals often have heightened sensory processing that can either intensify or overwhelm sexual experiences. Trauma survivors may find their amygdala stays activated even during arousal, making the "letting go" aspect more challenging.
Understanding your individual neurological wiring isn't about pathologizing differences - it's about working with your brain's specific patterns rather than against them.
The human sexual response cycle: Brain imaging evidence linking sex to other pleasures
II. The Neurochemical Timeline: Your Brain's Chemical Cascade
Your brain orchestrates sexual response through a precise sequence of chemical releases, each serving specific functions in building arousal, creating climax, and facilitating recovery.
Phase 1: Anticipation and Arousal (Dopamine Surge)
Dopamine floods your reward pathways, creating motivation and anticipation. This is your brain's "seeking" chemical - it drives you toward pleasurable experiences and makes you want more. You might notice your attention becoming more focused on sexual thoughts or sensations, increased excitement, and heightened motivation to pursue pleasure.
I notice this phase most clearly when I'm looking forward to intimate time with my partner. There's an anticipatory energy that builds throughout the day, making me more aware of physical touch, more responsive to flirting, more motivated to create the right conditions for intimacy.
This dopamine surge can build over hours or days with anticipation, then intensifies significantly during early arousal phases. It's the neurochemical foundation that makes you want to continue toward sexual experience.
Phase 2: Mounting Arousal (Multiple Neurotransmitters)
As arousal builds, norepinephrine increases focus and arousal while early oxytocin release begins the bonding process. Your brain starts suppressing analytical thinking while amplifying sensory processing.
This creates increased focus on physical sensations, decreased awareness of surroundings, and heightened sensitivity to touch. Mental chatter often quiets as physical sensation takes precedence. Some people experience this shift more dramatically than others - those with anxiety or busy minds might need more time or specific conditions to achieve this focused state.
For neurodivergent individuals, this transition may look different. ADHD brains, which typically have lower baseline dopamine, might need more intense or varied stimulation to achieve this focused state. Autistic individuals might experience sensory overwhelm instead of pleasant focus, requiring specific environmental modifications like softer lighting or particular textures.
Phase 3: Peak Response (The Neurochemical Flood)
The moment of orgasm triggers a massive release of multiple chemicals simultaneously:
Oxytocin: Often called the "bonding hormone," creates feelings of connection and emotional warmth. This explains why sexual experiences can dramatically affect how close you feel to your partner.
Endorphins: Natural opioids that create euphoria and pain relief. This is why orgasms can temporarily relieve chronic pain or tension headaches.
Prolactin: The satisfaction and contentment chemical that creates that deeply satisfied feeling after climax.
Endocannabinoids: Natural compounds similar to cannabis, creating bliss and relaxation.
This combination creates an altered state of consciousness that can feel spiritual, overwhelming, or profoundly connecting. The neurochemical flood often releases stored emotions - the same chemicals that create sexual pleasure also process emotional experiences, which is why you might laugh, cry, or feel unexpectedly emotional after intense orgasms.
Phase 4: Resolution and Afterglow (Prolactin and Recovery)
Prolactin levels spike, creating satisfaction and possible sleepiness. Dopamine gradually returns to baseline while the bonding effects of oxytocin can last for hours.
This phase brings contentment, reduced stress and anxiety, and continued emotional connection. I've noticed that the afterglow period significantly affects my stress resilience for the rest of the day. Good sex acts like a reset button for anxiety and overwhelm in ways that other relaxation techniques don't match.
-The Neuroscience of Orgasm: What Actually Happens in Your Brain
-The Science of the Female Orgasm How Pleasure Really Works
What happens in the brain during orgasm? These scientists dared to find out 🫣
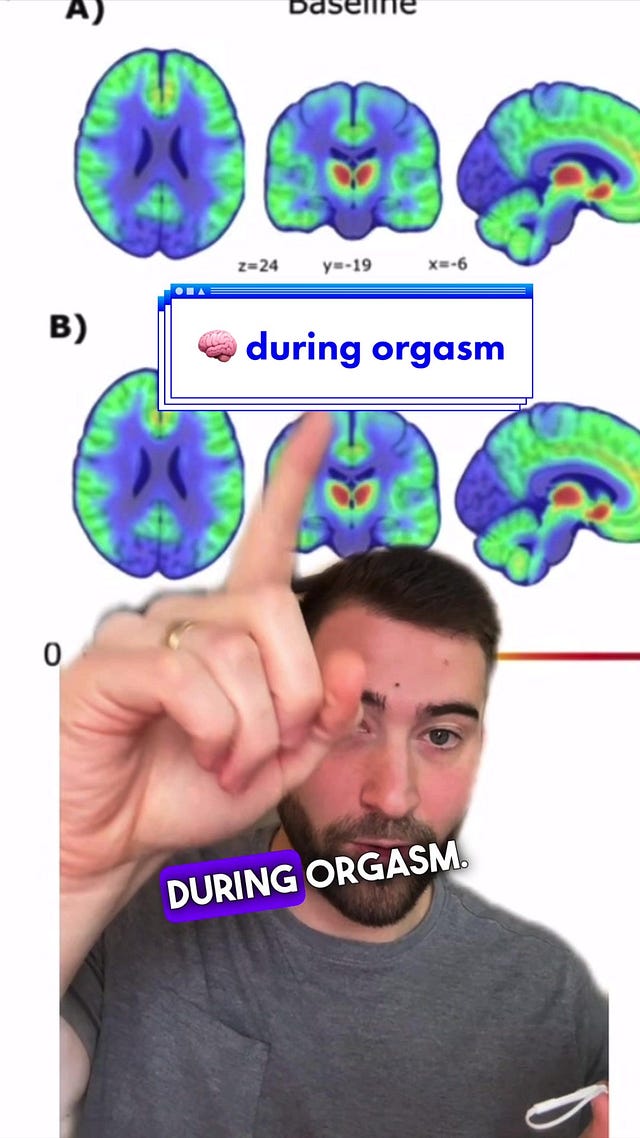
III. Your Brain During Orgasm: What Lights Up and What Goes Dark
Brain imaging studies reveal fascinating patterns in neural activation during sexual response that help explain why orgasm feels so different from other physical experiences.
Regions That Activate
The Reward Network: The same areas that respond to food, drugs, and other pleasures light up intensely during orgasm, including the nucleus accumbens and ventral tegmental area - your brain's primary reward circuits.
Sensory Processing Centers: Areas processing touch, pressure, and internal bodily sensations become hyperactive, explaining the intense physical awareness during sexual response.
Emotional Centers: The insula and anterior cingulate cortex, involved in emotional processing and empathy, show increased activity, explaining why orgasm often involves intense emotional experiences.
The hypothalamus, which plays a key role in releasing hormones like dopamine and oxytocin, is one of the regions of the brain that lights up during orgasm.
Source: BIG THINK
Regions That Go Quiet
Analytical Centers: The prefrontal cortex, responsible for planning, analyzing, and self-criticism, dramatically reduces activity. This is why you can't think your way through an orgasm - your analytical brain literally goes offline.
Fear Centers: The amygdala, your brain's alarm system, quiets down. This neural quieting is necessary for the vulnerability and surrender that orgasm requires.
Self-Awareness Networks: Areas involved in self-consciousness and social judgment show decreased activity, allowing for complete absorption in physical experience.
When Trauma Affects Neural Patterns
Trauma can disrupt the normal pattern of brain activation during sexual response. The amygdala may remain hypervigilant instead of calming, the prefrontal cortex might stay analytically active as a protective mechanism, and the insula's body awareness might be compromised by dissociative responses.
This doesn't mean fulfilling sexual experiences are impossible - it means the neurochemical journey might require different pathways, more time, or specific trauma-informed approaches to help the nervous system feel safe enough to surrender.
This pattern explains why mindfulness practices can improve sexual response - they train similar states of present-moment awareness with reduced analytical thinking..
IV. Hormonal Changes Across the Lifespan
Your neurochemical responses during sex don't remain constant throughout life. Understanding these changes can help you adapt and maintain satisfying sexual experiences through different life stages.
Menstrual Cycle Effects
Estrogen Peaks (Follicular Phase): Enhanced dopamine sensitivity makes sexual experiences potentially more rewarding, with increased lubrication and sensitivity.
Ovulation: Testosterone surge increases libido and sexual motivation. Many women report more intense orgasms during ovulation.
Luteal Phase: Progesterone can dampen sexual response in some women, though others report deeper, more emotionally intense experiences.
Tracking my cycle helped me understand why my sexual response varies so much from week to week. During ovulation, I need less stimulation and experience more intense responses. During my luteal phase, I need more time and different kinds of touch, but when I do reach orgasm, it often feels more emotionally satisfying.
Pregnancy and Postpartum
Pregnancy: Increased blood flow can intensify sensations for some women, while nausea and fatigue reduce interest for others. The hormone cocktail of pregnancy creates unpredictable responses.
Postpartum: Dramatic hormone shifts, especially if breastfeeding, can significantly reduce libido and orgasmic response. Prolactin (the nursing hormone) actively suppresses sexual hormones.
Menopause and Beyond
Perimenopause: Fluctuating hormones create unpredictable sexual responses. Some women report increased libido as pregnancy concerns disappear; others struggle with declining estrogen effects.
Postmenopause: Lower estrogen affects lubrication, tissue elasticity, and arousal patterns. However, neurochemical capacity for pleasure doesn't disappear with age, and sexual satisfaction can actually improve with proper support and adaptation.
Medical Conditions Affecting Hormonal Response
Thyroid Disorders: Both hyperthyroidism and hypothyroidism can dramatically affect sexual response through disrupted metabolism and hormone production.
PCOS: Polycystic ovary syndrome creates irregular hormone patterns that can affect sexual response unpredictably throughout the cycle.
Diabetes: Affects nerve function and circulation, potentially impacting both physical arousal and neurochemical responses.
Autoimmune Conditions: Chronic inflammation can suppress the hormonal axis and affect energy available for sexual response.
V. When Chemistry Gets Disrupted: Medications and Sexual Response
Understanding how medications affect your neurochemical response can help you make informed decisions and adjust expectations when necessary. Medication-induced sexual dysfunction is far more common than most people realize, affecting 25-73% of people taking various medications, yet it's rarely discussed proactively in medical settings.
SSRIs and Sexual Response: The Serotonin-Dopamine Balance
Selective serotonin reuptake inhibitors fundamentally alter the neurochemical balance that drives sexual response. By increasing serotonin availability, SSRIs can dampen dopamine activity - the primary driver of sexual motivation and arousal.
Specific Effects:
Delayed Orgasm: 60-70% of women experience significantly longer time to climax
Reduced Intensity: Even when orgasm occurs, the neurochemical flood may be blunted
Decreased Initiation: Reduced dopamine means less motivation to seek sexual experiences
Emotional Blunting: Some people report feeling disconnected from the emotional aspects of sex
Timeline of Effects: Sexual side effects typically appear within 2-8 weeks of starting SSRIs and may worsen before improving. Some people experience adaptation after 3-6 months, while others have persistent effects throughout treatment.
Management Strategies:
Timing Strategies: Taking medication after sexual activity (with doctor approval)
Medication Holidays: Carefully supervised breaks during treatment
Switching Medications: Wellbutrin, mirtazapine, or vortioxetine may have fewer sexual side effects
Adjunct Treatments: Some doctors prescribe small doses of dopamine-enhancing medications
This was a significant issue in my own life. After starting an antidepressant, my sexual response changed dramatically. Understanding that this was neurochemical, not psychological, helped me work with my doctor to find solutions through timing medications, weekend breaks (with medical supervision), or switching to medications with fewer sexual effects.
Hormonal Contraceptives: Disrupting Natural Cycles
Birth control pills alter the entire hormonal environment that supports sexual response, often in ways that aren't immediately obvious.
Mechanisms of Sexual Disruption:
Suppressed Ovulation: Eliminates the natural testosterone surge that drives mid-cycle libido
Reduced Free Testosterone: Many pills increase sex hormone-binding globulin, reducing available testosterone
Altered Brain Chemistry: Synthetic hormones may not activate the same neural pathways as natural hormones
Vaginal Changes: Reduced estrogen can affect tissue health and lubrication
Individual Variations: Some women experience minimal effects, while others notice dramatic changes in libido, arousal, and orgasmic response. The type of progestin in the pill significantly affects sexual side effects, with some formulations being much more likely to cause problems.
Alternatives to Consider:
Non-hormonal IUD: Copper IUD maintains natural hormone cycles
Lower-dose Pills: May reduce sexual side effects while maintaining contraceptive effectiveness
Different Progestins: Some synthetic progestins have less anti-androgenic activity
Barrier Methods: Allow complete preservation of natural hormone cycles
Blood Pressure Medications: Circulation and Nerve Function
Several classes of blood pressure medications can interfere with the vascular and neurological processes necessary for sexual response.
Beta-blockers: Can reduce heart rate response and limit blood flow to sexual organs. May also affect the sympathetic nervous system activation necessary for arousal.
Diuretics: Can reduce overall blood volume and affect circulation. Some diuretics also affect potassium levels, which impacts nerve function.
ACE Inhibitors/ARBs: Generally have fewer sexual side effects, but some people still experience reduced response.
Calcium Channel Blockers: May affect smooth muscle function in sexual organs, though effects vary significantly between individuals.
Working with Your Doctor: Blood pressure control is crucial for overall health, including sexual health, so stopping medications isn't usually advisable. However, switching between classes or adjusting dosages can often minimize sexual side effects while maintaining cardiovascular benefits.
Psychiatric Medications Beyond SSRIs
Antipsychotics: Can dramatically affect sexual function through multiple mechanisms - prolactin elevation, dopamine blockade, and sedation. Even newer "atypical" antipsychotics can cause significant sexual side effects.
Mood Stabilizers: Lithium can affect thyroid function and overall energy, while anticonvulsants used for mood stabilization (like valproate) can affect hormone levels.
Benzodiazepines: While anxiety reduction might theoretically improve sexual response, these medications often reduce overall arousal and can blunt emotional experiences during sex.
ADHD Medications: Stimulants can have variable effects - some people report improved focus enhances sexual experiences, while others find stimulants create too much mental activation to achieve the relaxed focus necessary for sexual response.
Pain Medications and Opioids
Short-term Pain Relief: Occasional use of NSAIDs or other pain relievers rarely affects sexual function and may actually improve sexual experience by reducing physical discomfort.
Chronic Opioid Use: Creates significant sexual dysfunction through suppression of the hypothalamic-pituitary-gonadal axis. This can lead to dramatically reduced testosterone and estrogen production, affecting every aspect of sexual response.
Gabapentin and Pregabalin: Commonly prescribed for nerve pain, these can affect the neurological pathways involved in sexual sensation and response.
Navigating Medication Effects: Practical Approaches
Having the Conversation: Sexual side effects are medical concerns that deserve the same attention as any other medication side effect. Come prepared with specific information about how your sexual response has changed.
Tracking Changes: Keep notes about timing, intensity, and specific changes in sexual response. This information helps doctors make informed decisions about medication adjustments.
Balancing Benefits and Risks: Sometimes the mental health benefits of a medication outweigh sexual side effects, but this should be a conscious choice made with full information, not a surprise consequence you're expected to endure.
Seeking Specialists: Consider consulting with healthcare providers who specialize in sexual medicine if your primary doctor isn't comfortable addressing these concerns.
Patience with Adjustments: Finding the right medication balance for both mental health and sexual wellness often takes time and multiple adjustments. This process requires patience and good communication with your healthcare team.
The key insight is that medication effects on sexuality are real, common, and often manageable with proper medical support. Your sexual wellness is a legitimate health concern that deserves attention and solutions, not just acceptance of side effects as inevitable.
While medications can significantly disrupt sexual neurochemistry, other substances we commonly use also interact with these same brain systems in complex ways.
VI. Substances and Sexual Neurochemistry: What Helps and What Hinders
Understanding how various substances interact with your sexual neurochemistry can help you make informed choices about what supports or undermines your sexual response.
Alcohol: The Double-Edged Sword
Low Doses (1-2 drinks): Can reduce social anxiety and inhibition by dampening amygdala activity, potentially making it easier to access aroused states. Some people find this helpful for overcoming performance anxiety.
Moderate to High Doses (3+ drinks): Alcohol is a nervous system depressant that impairs the precise neurological coordination necessary for orgasm. It also reduces REM sleep, affecting next-day hormone production.
Chronic Use: Regular heavy drinking can chronically suppress the hypothalamic-pituitary-gonadal axis, leading to persistent sexual dysfunction even when not actively drinking.
Cannabis: Complex Interactions
THC Effects: Interacts directly with the endocannabinoid system activated during orgasm. Many people report enhanced physical sensations and reduced anxiety, though some experience difficulty maintaining focus or reaching climax.
CBD Effects: May reduce anxiety without the psychoactive effects of THC, potentially helping with nervous system relaxation necessary for sexual response.
Individual Responses: Cannabis effects on sexual response vary dramatically between individuals and strains. Some people find it essential for accessing pleasure, while others find it interferes with the neurochemical cascade.
Caffeine and Stimulants
Moderate Caffeine: Can enhance focus and energy, potentially supporting the attentional aspects of sexual response.
Excessive Stimulants: Can create too much sympathetic nervous system activation, making it difficult to access the relaxed focus necessary for orgasm.
The Bottom Line on Substances
Your brain's natural neurochemical orchestra is remarkably sophisticated. While substances might temporarily enhance certain aspects of sexual response, they can also interfere with your brain's natural ability to create these experiences. The goal is supporting your natural neurochemistry rather than depending on external substances for sexual satisfaction.
With a clear understanding of both helpful and harmful substances, we can now focus on actively supporting our natural neurochemical processes for optimal sexual response.
VII. Optimizing Your Neurochemical Environment
Understanding your brain's chemistry during sexual response suggests practical approaches for supporting optimal function.
Lifestyle Factors That Support Sexual Neurochemistry (Quantified)
Exercise: 150 minutes of moderate exercise weekly or 75 minutes of vigorous activity increases dopamine sensitivity, improves circulation, and reduces cortisol. Even 20-30 minutes of movement on the day of sexual activity can enhance neurochemical response.
Sleep: 7-9 hours nightly for optimal hormone production. Sexual response suffers dramatically with less than 6 hours of sleep for more than a few days. REM sleep is particularly crucial for testosterone production.
Stress Management: Chronic stress elevating cortisol above 15-20 mg/dL consistently suppresses sex hormones. Daily stress reduction practices - even 10-15 minutes - can help maintain healthy cortisol rhythms.
Nutrition: Blood sugar fluctuations beyond 70-140 mg/dL affect neurotransmitter production. Severe calorie restriction below 1200 calories daily can shut down sexual function entirely within weeks.
Mindfulness and Sexual Response
Research shows that mindfulness practices can improve sexual function by training the same neural states that facilitate orgasm - present-moment awareness with reduced analytical thinking. Mindfulness trains your ability to focus on physical sensation rather than mental distraction, directly supporting the brain state changes necessary for sexual response.
Even simple breathing practices before sexual activity can help shift your brain into a more receptive state.
Troubleshooting: When to Seek Additional Support
Red Flags Requiring Medical Evaluation:
Complete loss of sexual interest lasting more than 3 months
Sudden changes in orgasmic ability without obvious cause
Physical pain during arousal or climax
Persistent inability to reach orgasm despite trying various approaches
Sexual response changes after starting new medications or medical treatments
When Lifestyle Changes Aren't Enough: If you've addressed sleep, exercise, stress, and nutrition for 2-3 months without improvement, consider underlying medical conditions, hormone imbalances, or the need for specialized sexual medicine consultation.
Trauma-Informed Approaches: If your nervous system seems unable to shift into the relaxed states necessary for sexual response, trauma-informed therapy, somatic experiencing, or EMDR might address underlying nervous system dysregulation that lifestyle changes alone can't resolve. As discussed in Section III, trauma can disrupt normal brain activation patterns during sexual response, keeping protective mechanisms active when vulnerability is needed.
These optimization strategies work best when we understand the broader implications of sexual neurochemistry for our overall wellbeing and relationships.
VIII. The Bigger Picture: Why Sexual Neurochemistry Matters
Understanding the brain science of sexual response isn't just interesting - it's empowering. When you know what's happening neurochemically, you can make informed medical decisions about medications that affect sexual response, reduce performance anxiety by understanding that your brain needs to shift out of analytical mode, and appreciate that neurochemical responses vary significantly between people.
This knowledge helped me integrate sexual wellness with overall health. Sexual activity produces neurochemicals that improve mood, reduce stress, and strengthen relationships, making sexual wellness a component of overall mental health care.
Partner Dynamics and Neurochemical Understanding
Understanding each other's neurochemical patterns can transform sexual communication. When you know your partner needs 20-30 minutes for their analytical brain to quiet, or that their medication affects their dopamine response, you can adjust timing and expectations accordingly.
Mismatched neurochemical patterns don't mean incompatibility - they mean needing different approaches. For example, I learned that my partner's ADHD medication affects their dopamine baseline differently than my natural cycle variations. Instead of feeling rejected when they needed more time or different stimulation, I understood this was neurochemical, not personal. Similarly, when I track my cycle and communicate that I'm in a phase where I need gentler touch but will likely have more emotionally intense responses, we can both adjust our approach and expectations.
The oxytocin bonding effects also explain why sexual frequency affects relationship dynamics beyond just physical satisfaction. Regular sexual connection literally rewires your brains for increased empathy and emotional attunement with each other.
Most importantly, understanding the bonding effects of oxytocin and the stress-relief benefits of sexual activity helped my partner and me appreciate why sexual connection affects relationship dynamics beyond just physical pleasure.
Your brain during sexual response is accomplishing something remarkable: creating physical pleasure, emotional bonding, stress relief, and even transcendent experiences through precise neurochemical orchestration. Understanding and honoring this process is a form of self-care that extends far beyond the bedroom.
Key Takeaways
Your sexual response is a sophisticated neurochemical symphony involving dopamine, oxytocin, endorphins, and other chemicals that affect your entire wellbeing
Individual variations are normal - neurodivergent brains, trauma histories, and life circumstances all influence how this system functions
Many medications significantly impact sexual neurochemistry - these effects are real, common, and often manageable with proper medical support
Lifestyle factors directly support sexual neurochemistry - adequate sleep, regular exercise, stress management, and mindful practices enhance your brain's natural capacity for pleasure and connection
Next up: In Issue 5, we'll explore "Out-of-Nowhere Orgasms" - the fascinating world of spontaneous and non-genital sexual responses, including the neurological pathways that make fantasy orgasms and exercise-induced climaxes possible.