Issue 1: Unlocking the Mysteries of Orgasm: A Deep Dive into the Anatomy of Pleasure
Section 1 | Purpose, Context & Why This Matters
Purpose & Context
Female orgasms remain among the most misunderstood, under-researched, and politicized aspects of human health. Across decades, medical research has overwhelmingly centered on reproduction and male sexual function, leaving vast blind spots in our knowledge of how the orgasmic experience actually works — especially for women, nonbinary individuals, and people of color.
This neglect isn’t accidental — it reflects deep cultural biases about whose pleasure is worth studying, whose bodies deserve understanding, and whose voices are believed.
The Cost of That Neglect
When anatomy is missing from sex education — or glossed over in medical training — it doesn’t just leave people uninformed; it creates a system where female sexual function is treated as optional, mysterious, or even suspect.
This gap fuels the orgasm gap:
In heterosexual relationships, 85–95% of men report climaxing during a sexual encounter, compared to just 64–65% of women.
That disparity narrows dramatically when women’s actual anatomical needs are met — proof that the issue is not biology alone, but also communication, sexual scripts, and access to accurate information.
Understanding this anatomy is not simply about “better sex.” It’s about:
Bodily autonomy — knowing how your own body works so you can advocate for it.
Hormone regulation — orgasms trigger oxytocin, endorphins, and dopamine that influence mood, bonding, and pain perception.
Trauma recovery — reconnecting with sensation can be part of reclaiming safety and self.
Health equity — ensuring that all people have access to both the knowledge and the care that make pleasure possible.
Your Pleasure Map
Knowing how your body is built is the foundation for:
1️⃣ Mapping what feels good so you can find it again — solo or partnered.
2️⃣ Communicating with partners clearly and confidently, replacing guesswork with specifics.
3️⃣ Reclaiming intimacy in a culture that too often treats female pleasure as secondary to performance.
⚖️ Equity Call-Out
The erasure of female anatomy from textbooks and curricula is not just ignorance — it’s structural inequality. Closing that knowledge gap is part of closing the orgasm gap, and it’s a direct act of reproductive justice.
Why This Matters 💡
Picture a quiet moment — alone or with someone you trust — where there’s no rush. You notice the softness of the sheets, the way your breath deepens, the hum of curiosity beneath your ribs. This is where pleasure begins: not with performance, but with awareness. And awareness starts with knowing how your body actually works.
Female orgasm is not just a perk or a bonus — it’s a lens into autonomy, health equity, and the right to know your own body. For much of modern medical history, women’s sexual response has been treated as a mystery, a luxury, or an afterthought. Research dollars and clinical training have overwhelmingly prioritized erectile function, penile blood flow, and male sexual performance. Meanwhile, women have been left with cultural scripts — from romance novels to porn — that almost never align with real physiology.
The result is a cascade of myths:
That penetration alone should “do the trick” 🚫
That women who take “too long” are broken ⏳
That pleasure is optional if everything else in the relationship looks good on paper 📝
These messages aren’t harmless. They shape expectations, influence how partners behave in bed, and even affect the kinds of medical care women receive when they raise concerns about arousal or orgasm.
The Truth 📊
The truth is both simpler and more radical: the majority of women need clitoral stimulation to reach orgasm — somewhere between 70% and 90%, depending on the study — and that’s neither a flaw nor a failure. It’s anatomy.
When that anatomy is acknowledged and integrated into sexual experiences, the “orgasm gap” shrinks dramatically:
In heterosexual encounters: 85–95% of men climax vs. 64–65% of women.
In encounters between women: the number jumps to 86%.
💡 This proves the gap is about knowledge and technique, not biology.
The Health Stakes ❤️🩹
There are also tangible health stakes. Orgasms trigger surges in oxytocin and endorphins, relaxing the nervous system, easing pain, improving sleep, and enhancing mood. Pelvic floor contractions during climax help maintain muscle tone and circulation, which supports bladder and bowel function.
Evidence shows regular orgasmic activity can:
Support cardiovascular health 🫀
Reduce stress hormone levels 🌀
Improve immune response 🛡️
Far from being frivolous, pleasure is part of a holistic model of health.
When Pleasure Feels Out of Reach 🚨
Conversely, difficulty or inability to climax — known as anorgasmia — can signal underlying issues:
Hormonal changes from menopause or postpartum shifts.
Medication effects (50–70% of SSRI users report sexual side effects).
Pelvic floor dysfunction.
Chronic stress or unresolved trauma.
These aren’t problems to “just get over.” They’re signals from the body that deserve attention, compassion, and, when needed, medical support.
The Equity Factor ⚖️
Finally, this matters because inequity runs through the data. Access to pelvic floor therapy, sexual counseling, and accurate sexual anatomy education is uneven:
Black women are more likely to have sexual pain dismissed or misdiagnosed.
Trans and nonbinary individuals may face both provider knowledge gaps and lack of affirming care.
Closing the orgasm gap isn’t just about bodies — it’s about power, justice, and the refusal to accept less when more is possible.
The Orgasm Gap (And Why It’s Not Your Fault) ⚖️
The numbers tell a clear story: there’s a consistent, measurable difference between how often men and women orgasm in heterosexual encounters — and it has nothing to do with women being “broken” or “too slow.” It has everything to do with anatomy, scripts, and whether real needs are being met.
What the Data Shows 📊
Penetration Alone:
Only about 18% of women climax reliably from vaginal penetration by itself. The vast majority — roughly 80% — need direct or indirect clitoral stimulation to reach orgasm.
Partnered Sex:
In heterosexual encounters:
Men: orgasm ~90–95% of the time.
Women: orgasm ~60–70% of the time.
That gap narrows dramatically when clitoral stimulation (manual, oral, toys) is part of the routine.
Orientation Differences: Lesbian couples report far higher orgasm consistency — often 80–90% — showing that technique, communication, and the scripts you follow matter just as much as biology.
Timing: Women’s typical time-to-orgasm in partnered sex spans anywhere from 4 to 25+ minutes of consistent stimulation. Solo exploration often takes less time. Timing shifts with:
Context and partner dynamics
Stress levels
Menstrual cycle phase
Type of stimulation used
Myth-Busting the “Right” Kind of Orgasm 🛑
🚫 Myth: “Vaginal orgasms” are separate and superior.
✅ Fact: Internal and external routes converge on the clitoral network. Different paths, same system.
🚫 Myth: If penetration “isn’t enough,” you’re broken.
✅ Fact: For most women, penetration alone is not enough — and that’s normal.
Health Benefits (Beyond the Bedroom) ❤️🩹
Orgasms are not just pleasurable — they have measurable physiological benefits:
Pelvic Health 🏋🏽♀️ — Rhythmic pelvic-floor contractions during climax strengthen muscle tone and coordination, supporting bladder control, bowel health, and core stability.
Stress & Mood 🌿 — Post-orgasm spikes in oxytocin and endorphins can lower stress reactivity, lift mood, and ease pain.
Sleep & Relaxation 😴 — After climax, the body often shifts into parasympathetic dominance (“rest and digest”), helping sleep onset and improving rest quality.
Bonding & Connection 🤝 — Oxytocin boosts trust, closeness, and emotional regulation — deepening intimacy.
Cycle & Hormones 🔄 — Orgasms can reduce perceived PMS symptoms. Perimenopausal arousal changes can often be improved with local estrogen, high-quality lubricants, and pelvic therapy, preserving orgasm quality well into later life.
Persistent difficulty or inability to climax — anorgasmia — can stem from:
Medication effects (50–70% of SSRI users report sexual side effects).
Hormonal shifts (menopause, postpartum).
Pelvic-floor dysfunction.
Chronic stress or unresolved trauma.
These are not personal failings. They are signals that can be addressed with the right support.
Quick Guide: When to Seek Help 🩺
Red Flags to Evaluate:
Ongoing difficulty or absence of orgasm ≥ 6 months with distress.
New changes after childbirth, surgery, or starting a new medication.
Pain, numbness, or marked hypersensitivity that blocks pleasure.
Where to Start:
Clinical Care 🩻 — Medication review (especially SSRIs, hormonal methods), pelvic exam, lab work if needed.
Pelvic-Floor PT 🧘🏽♀️ — For weakness, hypertonicity, scar tissue, or pain with sex.
Counseling/Coaching 🗣 — Mindfulness to address distraction/performance anxiety, trauma-informed therapy, and communication skills training.
Power Note: Closing the knowledge gap is how we close the orgasm gap. This is not about asking for “extra” — it’s about reclaiming your anatomy, rewriting your sexual script, and getting the care you deserve.
Section 2 | External & Internal Genital Anatomy 🔍
Closing the orgasm gap starts with knowing exactly what’s under your skin — the full anatomy that powers arousal, pleasure, and climax.
Most of us were taught — in school, in casual conversation, even in medical settings — that the vulva is “the vagina.” In reality, the vagina is just one part of a much larger and more intricate pleasure system. Closing the orgasm gap starts here, with a clear, accurate map of both the parts you can see and the hidden structures that make orgasm possible.
External Structures 🌸
These are the parts you can see and touch, each contributing to sensation in different ways:
Labia Majora & Labia Minora — The outer and inner folds of skin that frame the vulva. Both are rich in nerve endings and blood vessels, and they respond visibly to arousal, swelling and deepening in color. The labia minora, in particular, can be highly sensitive to touch, warmth, and pressure.
Clitoral Glans — The small, visible “button” beneath the clitoral hood is actually just the tip of a much larger erectile organ. Containing approximately 8,000 sensory nerve endings — about double the number in the penis — the glans is exquisitely responsive to light touch, vibration, and temperature changes.
Urethral Opening — Often ignored in sexual anatomy discussions, this is where urine exits the body. It lies just below the clitoral glans and can be indirectly stimulated by touch to the surrounding tissue, contributing to arousal for some people.
Vaginal Opening (Introitus) — The entry to the vaginal canal, surrounded by nerve-rich tissue that can contribute to blended orgasms when combined with clitoral stimulation.
Perineum — The stretch of skin between the vaginal opening and anus. It’s sensitive to pressure and is often engaged during orgasmic contractions, adding to overall sensation.
External view of the vulva — Depicts the mons pubis, labia majora and minora, clitoral glans and prepuce, urethral and vaginal openings, hymen, and the greater vestibular (Bartholin’s) glands. Also shows the bulb of the vaginal vestibule beneath the surface. Source: An overview of the female reproductive.
Internal Structures 💗
Beneath the surface lies the hidden bulk of the sexual pleasure system — erectile tissue, nerve networks, and glands that work together during arousal and orgasm:
Clitoral Crura — Internal “legs” of erectile tissue that extend from the glans down and around the vaginal canal like a wishbone. During arousal, they swell with blood, increasing sensitivity to internal movement and pressure.
Vestibular Bulbs — Paired, elongated cushions of erectile tissue located beneath the labia minora. They swell during arousal, creating a “full” feeling and amplifying pressure against the vaginal walls.
Vaginal Canal — A muscular, adaptable tube that can indirectly stimulate the internal clitoral structures when touched, penetrated, or moved against. Its front wall contains part of the internal clitoral network.
Skene’s Glands — Located near the urethra, these glands may play a role in fluid release during orgasm (sometimes referred to as “female ejaculation”), though their function and significance are still under-researched.
G-Spot Zone — More accurately described as the anterior vaginal wall’s nerve-rich region, not a discrete organ. For some people, stimulation here (often combined with external clitoral touch) produces deep, throbbing pleasure.
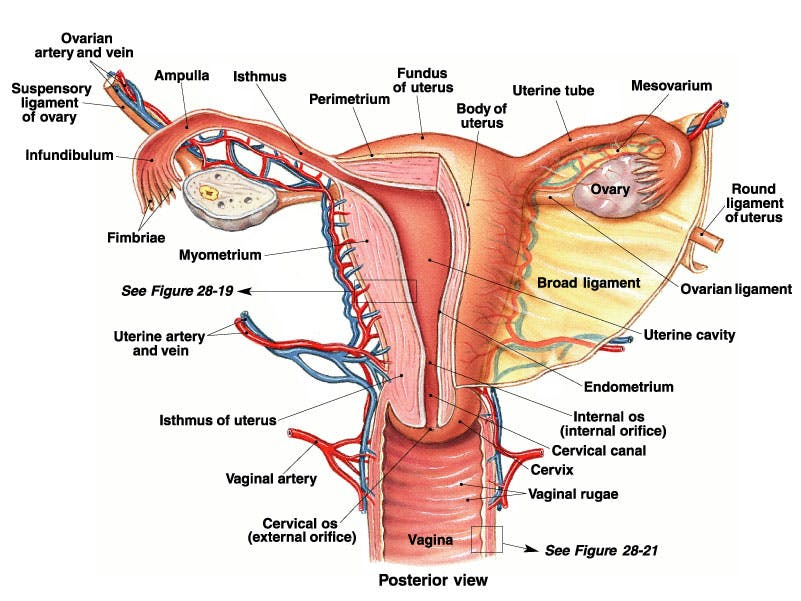
Posterior view of the female reproductive system — Shows the uterus, ovaries, fallopian tubes, cervix, vagina, and associated ligaments, arteries, and veins. Highlights the structural relationships between reproductive organs and surrounding vasculature.
Source: Female Reproductive System Drawing – GetDrawings.com
Sagittal (side) view of the female pelvis — Illustrates internal reproductive organs (ovaries, uterus, cervix, vagina) in relation to surrounding structures such as the bladder, rectum, and pubic bone. Labels erectile tissues, Skene’s glands, G-spot zone, and vulvar anatomy.
Source: Female Reproductive System Drawing – GetDrawings.com
📊 Research Insight
Orgasmic capacity can be influenced by anatomy. One notable finding: the shorter the distance between the clitoral glans and vaginal opening (known as the clitoral–urethral–vaginal distance), the more easily some people may experience blended orgasms from penetration and clitoral stimulation combined.
Section 3 | The Full Clitoral Complex 🔬
For much of modern medical history, the clitoris was depicted in textbooks as little more than a small external nub — a pink dot on a diagram, barely labeled, and often ignored entirely in sexual health discussions.
This error of omission shaped not only public understanding of women’s pleasure but also clinical practice, leaving providers ill-equipped to address sexual function holistically.
Modern imaging has finally corrected the record: the clitoris is an expansive, wishbone-shaped organ measuring roughly 9–11 cm in total length, with most of its structure hidden beneath the surface. Far from being a minor appendage, it is a complex network of erectile tissue, nerves, and vascular structures designed for pleasure.
💡Key Components of the Clitoral Complex
Glans — The visible external part, located beneath the clitoral hood. Packed with over 8,000 sensory nerve endings (about twice the number in the penis), the glans is highly responsive to light touch, vibration, and changes in temperature or pressure.
Shaft — A short, hidden segment that connects the glans to the deeper structures, transmitting sensation inward.
Crura (“legs”) — Two elongated arms of erectile tissue that extend down and curve around either side of the vaginal canal, anchoring the clitoris to the pubic bone. These swell with blood during arousal, enhancing internal pressure sensation.
Vestibular bulbs — Paired masses of erectile tissue beneath the labia minora. During arousal, they engorge and press against the vaginal walls, increasing friction and amplifying sensation.
💡 MRI Breakthroughs
In the early 2000s, pioneering research by Dr. Helen O’Connell and colleagues used 3D magnetic resonance imaging to reveal the true size, shape, and depth of the clitoral complex. These scans confirmed that most so-called “vaginal” orgasms are actually mediated by clitoral tissue — even when the stimulation feels internal.
🚫 Myth Busted
The idea of “clitoral orgasms” vs. “vaginal orgasms” as separate and hierarchical is a false binary. Internal and external routes stimulate the same organ through different access points. Whether the sensation is localized to the glans, the vaginal walls, or a blended experience, the clitoral network is engaged.
📊 Research Insight
The clitoris is purely dedicated to pleasure — it has no direct reproductive function. Its structure is homologous to the penis, but unlike the penis, its erectile tissue and nerve density are optimized for sensation rather than penetration or urination.
MRI-enhanced anatomical view of the clitoral complex in situ, illustrating how the glans, shaft, crura, and vestibular bulbs align with surrounding pelvic structures. (Source: recent 3D MRI data — American Journal of Obstetrics & Gynecology tutorial.)
-Female orgasm | Female anatomy and biology
Section 4 | Pelvic Floor Muscles 🏋🏽♀️
The pelvic floor is a hammock-like network of muscles stretching from the pubic bone to the tailbone, supporting the bladder, uterus, and rectum. Far from being just a structural support system, these muscles are active participants in sexual pleasure. During orgasm, they contract rhythmically — usually about every 0.8 seconds — intensifying sensation, deepening pleasure, and sometimes aiding in fluid release or ejaculation.
Strong, well-coordinated pelvic floor muscles (PFMs) can enhance orgasmic quality, creating more intense, pulsing contractions that feel like waves rolling through the pelvis. Conversely, PFMs that are weak, injured, or hypertonic (overly tight) can blunt sensation or even cause discomfort during arousal or orgasm.
Common causes of pelvic floor changes include:
Vaginal childbirth (especially with tearing or instrumental delivery)
Pelvic surgery (including hysterectomy or episiotomy)
Menopause and hormonal changes
Chronic stress or trauma that keeps the muscles in a constant state of tension
📊 Evidence: Clinical trials show pelvic floor muscle training (PFMT) can improve orgasm quality in up to 80% of participants — especially when combined with biofeedback or guided physiotherapy.
Recovery & Optimization Tools
PFMT (Kegels) with or without biofeedback devices
Scar tissue release after surgery or birth
Trauma-informed pelvic therapy to address emotional and physical tension
Breathwork to release hypertonicity and improve coordination
Beyond Kegels: Why Orgasms Might Be the Ultimate Pelvic Workout 💥
While Kegels are a well-known way to strengthen the pelvic floor, orgasms may actually provide a more complete and powerful workout.
Why:
Orgasms recruit more muscle fibers and trigger involuntary, coordinated contractions that most people can’t achieve with voluntary Kegels.
These contractions are rhythmic and multidirectional, working several pelvic muscles at once.
Neurological activation during orgasm increases blood flow, oxygenation, and nerve sensitivity in ways Kegels alone do not.
💡 Pro Tip: Some pelvic floor therapists recommend incorporating regular orgasms — solo or partnered — into a pelvic health routine, especially for those who struggle with motivation for daily Kegels.
Myth-Busting: Orgasm & Fertility 🍼
🚫 Myth #1: You need to orgasm to get pregnant.
✅ Fact: Pregnancy can occur without orgasm. Fertilization is about sperm meeting egg, which doesn’t require climax.
🚫 Myth #2: Orgasms have nothing to do with fertility.
✅ Fact: While not required for conception, orgasms may help. Rhythmic pelvic floor contractions can create an “upsuck effect” that helps sperm travel toward the cervix. Post-orgasm relaxation may also improve cervical mucus quality, making it easier for sperm to survive.
Pelvic floor muscles of the female pelvis, viewed from below. This diagram shows key muscle groups — including the puborectalis, pubococcygeus, iliococcygeus, and coccygeus — along with openings for the urethra, vaginal canal, and rectum. These muscles support pelvic organs and play a central role in orgasmic contractions, continence, and core stability.
-Female-pelvic-floor-muscle-3D-animation
-Science Explains How Orgasms Might Be Better Than Kegel Exercises
-Wondering what happens to a female body during orgasm.
Section 5 | Neural Pathways to Orgasm 🧠
Pleasure is not just a local event — it’s a full-body symphony, with the brain as the conductor and the nervous system as the orchestra. The genital region is wired into the brain through four major sensory highways, each delivering its own flavor of sensation. These networks overlap and reinforce each other, which is why stimulation in one area can intensify or transform sensation elsewhere.
The Four Orgasm Highways 🚦
Pudendal nerve — Transmits signals from the clitoris, vulva, labia, and perineum. Highly responsive to light touch, pressure, and vibration, it’s often the star in external clitoral stimulation.
Pelvic nerve — Carries sensation from the vaginal walls and nearby erectile tissue. Often engaged during penetration and indirect clitoral stimulation.
Hypogastric nerve — Relays input from the cervix and uterus, often linked to deep, spreading orgasmic sensations that can feel more internal or emotional.
Vagus nerve — The wildcard. Unlike the others, it bypasses the spinal cord entirely, sending signals directly to the brainstem. This makes it possible for some people with complete spinal cord injuries to experience orgasm through deep vaginal or cervical stimulation.
Beyond the Genitals 🔍
Not all orgasms require direct genital touch. Because the brain is the ultimate processing hub, sensations from other areas can merge with erotic pathways:
Nipple stimulation — Activates the same brain regions as genital touch.
Erotic fantasy or emotional arousal — Mental imagery, anticipation, and memory can trigger physical responses without direct contact.
Deep pressure points — Certain areas of the body (e.g., inner thighs, behind the knees) can tap into erotic neural circuits.
Rhythmic breathing or movement — Techniques like tantric breathing can heighten parasympathetic activation, tipping the body toward orgasm.
Sound and vibration — Low-frequency resonance can activate mechanoreceptors linked to pelvic nerves.
Why This Matters for Pleasure Mapping 🗺️
The diversity of pathways means your orgasmic potential is far broader than most sex education covers. You’re not limited to one type of touch or position — experimenting with different sensory routes can expand what’s possible.
It also explains why some people notice major changes in pleasure after injury, surgery, or childbirth: when one pathway is compromised, others can often be strengthened or recruited.
💡 Tip: Think of your erotic network like a city’s transit system — if one train line is closed, you can still reach the destination by taking another route.
Clinical Insights & Recovery Pathways 🩺
Understanding these nerve routes is more than an anatomy lesson — it’s a tool for troubleshooting changes in sensation or orgasmic function:
Post-surgery changes (e.g., hysterectomy, pelvic repair) can sometimes reduce stimulation along one pathway while leaving others intact. Pelvic floor physical therapy or intentional retraining of alternative routes can help restore pleasure.
Hormonal changes (menopause, postpartum) can alter tissue elasticity and nerve responsiveness, particularly in the pelvic and hypogastric pathways. Topical estrogen, adequate lubrication, and increased foreplay time can help re-sensitize these routes.
Neurological conditions (multiple sclerosis, spinal cord injury, neuropathies) can impact one or more pathways. Identifying which are still functional allows targeted stimulation techniques — for example, emphasizing vagus nerve activation in SCI (spinal cord injury) patients.
Myth-Bust Corner 🛑
🚫 Myth: “If you can’t orgasm from penetration alone, you’re doing it wrong.”
✅ Fact: Penetrative sex primarily stimulates the pelvic and hypogastric nerves, which often need to work in concert with the pudendal pathway for orgasm.
🚫 Myth: “Orgasms are all about the genitals.”
✅ Fact: They’re about neural convergence — the merging of multiple sensory inputs in the brain’s pleasure centers. That’s why nipple play, fantasy, or even a whispered word can sometimes send someone over the edge.
Reader Takeaways 💡
Your orgasmic network has multiple access points — explore them.
Neural diversity means pleasure can be adapted, expanded, and rediscovered after life changes.
The brain is as important as the body in creating orgasm — mental and emotional context shape the intensity and quality of climax.
Section 6 | Blood Flow & Engorgement 💗
Arousal is as much a vascular process as it is a neural one. When you become sexually aroused, vasocongestion — the pooling of blood in genital tissues — causes swelling, warmth, and heightened sensitivity. This surge in circulation is what makes tissues more responsive to touch and movement, setting the stage for orgasm.
What Happens During Arousal 🔬
As blood flow increases, erectile tissue in the genitals reacts in ways that can be felt, seen, and even measured:
Clitoral glans, crura, and vestibular bulbs — These erectile structures swell, become firmer, and more prominent under the skin, amplifying sensitivity.
Vaginal walls — Take on a deeper pink or purplish hue due to increased blood volume.
Labia minora — Swell and may visibly change color, a sign of heightened arousal.
Lubrication begins — Plasma seeps through the vaginal walls in a process called transudation, creating natural moisture that can make touch and penetration more comfortable.
📊 Important Note: Arousal ≠ Desire
Your body can be physiologically “ready” without you feeling mentally or emotionally in the mood — and vice versa. This is sometimes called arousal–desire mismatch and is a normal variation, but it can become a source of confusion or strain in relationships if not understood. Recognizing that physical readiness and emotional readiness aren’t always aligned can help improve both communication and consent practices.
Factors That Influence Blood Flow & Arousal ⚖️
Blood flow is sensitive to changes inside and outside the body. Factors that can speed it up, slow it down, or block it entirely include:
Hormonal shifts — Menstrual cycle phases, pregnancy, postpartum recovery, and menopause can all change genital blood flow.
Stress, fatigue, or anxiety — Stress hormones like cortisol can constrict blood vessels, reducing engorgement.
Cardiovascular health — Conditions like atherosclerosis, diabetes, or high blood pressure can impact circulation to the pelvic region.
Medications — Some antidepressants (SSRIs), antihypertensives, and hormonal contraceptives can reduce genital blood flow or alter lubrication.
Why Blood Flow Matters for Pleasure 💡
Strong, healthy circulation to the pelvic region doesn’t just improve sensation — it supports tissue health over time. Increased blood flow brings oxygen and nutrients to genital tissues, helping maintain elasticity, responsiveness, and overall function. This is one reason why regular sexual activity — solo or partnered — can contribute to long-term sexual wellness.
Section 7 | Orgasm Typology: Body Maps of Pleasure 🗺️
There is no hierarchy of “better” or “more mature” orgasms — all types are valid and, anatomically, all involve the clitoral network in some way. What changes from one orgasm type to another is how stimulation reaches that network, which nerves are most engaged, and how the experience is processed in the brain and body.
Think of it like music — the clitoral network is the instrument, but different styles of touch, pressure, and context create entirely different songs.
The Main Orgasm Types 🎶
Clitoral ✨ — The most common orgasm type, achieved through direct stimulation of the clitoral glans or indirect stimulation via the shaft and hood. With roughly 8,000 sensory nerve endings in the glans alone, sensations are often sharp, focused, and localized — but they can ripple through the pelvis, abdomen, and even the legs.
Vaginal 🌊 — Usually a blended response involving indirect activation of the internal clitoral structures (crura, bulbs) through penetration, movement, and pressure against the anterior vaginal wall (the so-called G-spot zone). Feels deeper and more diffuse, sometimes building more slowly but lasting longer.
Cervical 💫 — Deep, often emotionally intense sensations that can radiate through the pelvis and spine. Requires stimulation of the cervix, often via specific angles or positions, and for many, a state of full trust, relaxation, and arousal. Cervical orgasms may trigger strong aftershocks or even tears, given their connection to the hypogastric nerve.
Anal 🔥 — Activates pudendal nerve endings located in and around the anus, which connect to the same orgasmic circuitry as the genitals. Can be intensely pleasurable and full-body for some, but requires communication, preparation, and a focus on relaxation and lubrication.
Blended 🌈 — Combines two or more stimulation routes (e.g., clitoral + vaginal, clitoral + anal), often producing the most intense and long-lasting orgasms because multiple nerve networks are firing at once.
Nipple Orgasms 💗 — Stimulate the same brain regions as genital orgasms via the vagus nerve. Sensations can be surprisingly full-body and, for some, trigger simultaneous clitoral or blended orgasms without genital touch.
🚫 Myth Busted: The Freud Fallacy
Myth: Vaginal orgasms are “mature,” while clitoral orgasms are “immature.”
Fact: This early-20th-century claim by Freud has been debunked repeatedly. Internal and external stimulation are not in competition — both routes ultimately activate the same clitoral network. The difference is location and sensation, not legitimacy.
Why This Matters for Pleasure Mapping 🗺️
Recognizing that all orgasms are variations of the same core system frees you from outdated sexual hierarchies. This knowledge opens the door to curiosity without shame — an invitation to experiment, mix pathways, and discover what lights up your nervous system.
💡 Tip: Keep a pleasure map journal tracking which types of stimulation work best for you in different contexts — solo, partnered, relaxed, stressed, during different points in your cycle, or after specific life events (e.g., childbirth). Over time, you’ll see patterns emerge that help you customize your sexual experiences for maximum satisfaction.
Section 8 | Comparative Physiology ⚖️
When comparing orgasm physiology across sexes, there are both fascinating overlaps and striking differences. Understanding these differences isn’t about competition — it’s about appreciating how bodies respond, what they need, and how context shapes the experience.
Latency: The Time to Climax ⏳
Women — During partnered sex, orgasm typically occurs after 10–20 minutes of consistent, pleasurable stimulation. Solo exploration is often faster, averaging 8–12 minutes, since there’s no need for partner coordination and the individual can focus directly on what feels best.
Men — In partnered encounters, the average time to climax is 5–7 minutes; during solo masturbation, it’s even shorter at 4–5 minutes.
💡 Why this matters: Sexual scripts that treat men’s average timing as “the norm” often leave women’s needs unmet unless intentional adjustments are made.
Refractory Period: The Reset Interval 🔄
Women — Typically have no fixed refractory period, meaning they can experience multiple orgasms in quick succession if stimulation continues and remains pleasurable. This is due to the absence of a neurochemical “off switch” equivalent to that found in most male orgasm responses.
Men — The refractory period — the time after orgasm when arousal and orgasm are not physiologically possible — varies greatly. Younger men may be ready again within minutes, while older men may need several hours or even days.
Variability & Context Sensitivity 🌿
Women’s orgasms are more context-sensitive, shaped by:
Emotional connection — Trust and intimacy can increase relaxation, reduce anxiety, and heighten arousal.
Environment — Privacy, comfort, and a sense of safety can dramatically influence whether orgasm feels within reach.
Mental focus — The ability to tune out distractions, body image concerns, or performance pressure often determines how easily climax can occur.
Men’s orgasms tend to be less dependent on context in the short term but can still be affected by psychological factors such as stress, relationship dynamics, and self-confidence.
Reader Takeaways 💡
Differences in timing, recovery, and variability are not about one sex being “better” at orgasm — they reflect different biological wiring.
Aligning sexual activities with each partner’s natural rhythm (e.g., starting with more clitoral stimulation before penetration) can close the timing gap.
The lack of a fixed refractory period in women offers unique opportunities for multiple orgasms, provided comfort, arousal, and emotional safety are maintained.
Section 9 | Impact of Trauma, Birth & Surgery 🩹
Life events can reshape the landscape of sexual sensation — sometimes in subtle, barely noticeable shifts, and sometimes in dramatic, body-altering ways. These changes may be temporary and reversible with time and gentle care, or they may require intentional strategies to adapt and restore pleasure.
It’s important to remember: these experiences are not signs of “failure” or “loss.” They are evidence that your body and nervous system have been through something significant — and, with the right support, pleasure can evolve, return, and even deepen.
How Life Events Affect Orgasm 🔍
Childbirth 🍼 — Vaginal tearing, episiotomy, or C-section incisions can disrupt nerve pathways, create scar sensitivity, and alter muscle coordination. Even after physical healing, the nervous system may need time — and sometimes retraining — to reconnect sensation. Hormonal changes during postpartum (especially lower estrogen) can also impact lubrication, elasticity, and arousal.
Pelvic Surgery 🏥 — Procedures such as hysterectomy, prolapse repair, or incontinence surgery may alter muscle tone, shift pelvic organ positioning, or create scar tissue that changes how pressure and touch are perceived.
Trauma (Physical or Sexual) 💔 — Trauma can affect both the body’s ability to generate sensation and the mind’s ability to relax into pleasure. Survivors may experience increased tension, numbness, or delayed arousal responses — all of which are normal, valid reactions to lived experience.
💬 Affirmation: “If you’ve ever said, ‘I just don’t feel the same after childbirth,’ you are not imagining it — and there are paths to recovery.”
Recovery Tools & Pathways 🧰
Scar Desensitization Therapy — Gentle, progressive touch or massage techniques designed to retrain the nerves and restore sensitivity in scarred areas.
Perineal Massage — Improves circulation, flexibility, and tissue mobility in postpartum or post-surgery tissue.
Pelvic Floor Muscle Training (PFMT) — Restores tone, improves orgasmic intensity, and helps re-coordinate muscles that may have weakened or tightened after surgery or trauma.
Trauma-Informed Sexual Therapy — Combines emotional safety, trust-building, and physical re-engagement, ensuring that recovery addresses both mind and body.
Myth-Bust Corner 🛑
🚫 Myth: “Once sensation changes after birth or surgery, there’s nothing you can do.”
✅ Fact: Nerves can regenerate, muscles can be retrained, and pleasure pathways can be remapped — with the right combination of physical therapy, hormonal support, and emotional care.
Section 10 | Equity & Variation in Anatomy ⚖️
Pleasure is not evenly distributed — not because some bodies are “better” or “worse,” but because social systems, medical training, and access to care are not built equally for everyone. Your anatomy exists within a cultural and healthcare context that can either support or limit your ability to experience full, satisfying orgasms.
Understanding these inequities is essential. It shifts the conversation from “What’s wrong with me?” to “What barriers are shaping my experience — and how can they be removed?”
Factors That Shape Pleasure
Menopause 🌙 — As estrogen levels decline, vaginal tissue can become thinner, drier, and less elastic (atrophy). This can make arousal and orgasm more difficult or uncomfortable. Solutions exist — high-quality lubricants, vaginal moisturizers, and low-dose topical estrogen can restore comfort, increase blood flow, and maintain orgasmic potential well into later life.
Racial Inequities ✊🏾 — Black women are statistically less likely to receive referrals for pelvic floor therapy or sexual pain evaluation, despite having higher rates of birth trauma, fibroids, and chronic pelvic pain. This disparity is not due to biology but to systemic bias in medical care.
Trans & Nonbinary Experiences 🌈 — Hormone therapy and gender-affirming surgeries can shift arousal patterns, change tissue sensitivity, or alter which pathways are most effective for orgasm. For example, testosterone can increase libido but may also reduce natural lubrication; estrogen can enhance clitoral sensitivity but may require different stimulation techniques post-surgery.
🩺 Callout: “Most OB/GYNs never learn the full anatomy of the clitoris — even during residency.” This lack of training reinforces the pleasure gap and delays access to effective, affirming care.
Why This Matters 💡
When we acknowledge variation and inequity, we make space for care plans that are personal, precise, and just. It means no one is told, “That’s just how it is,” when what they need is evidence-based treatment, culturally competent care, and tools tailored to their unique anatomy and identity.
Section 11 | Reader Takeaways & Call-to-Action 💡
Understanding your sexual anatomy is not indulgent — it’s a radical act of self-care and self-advocacy. Pleasure is woven into health, identity, and autonomy. Knowing your body allows you to claim all three and to push back against the cultural scripts that have kept female pleasure in the shadows.
When you understand your orgasmic anatomy, you’re not just learning “what feels good” — you’re building a toolkit for:
Advocating for better healthcare
Improving communication with partners
Spotting and addressing changes early
Expanding your erotic possibilities at every life stage
Your Next Four Steps 🚀
1️⃣ See Your Anatomy Clearly — Use a mirror, a body-safe camera, or an anatomy app to explore your clitoral structure and surrounding pleasure zones. Understanding the landscape is the first step toward mapping it.
2️⃣ Track Your Pleasure Patterns — Pay attention to what works for you: specific types of touch, rhythm, pressure, positions, or mental imagery. Note the contexts that help or hinder — stress levels, emotional safety, or even time of day.
3️⃣ Reframe Your Expectations — Remember: 70–90% of women require clitoral stimulation to orgasm. This is the norm, not the exception. There is no “failure” in needing what your anatomy requires.
4️⃣ Ask for Support When Needed — Go into medical appointments with clarity and specificity. Example questions:
“Could pelvic-floor therapy help me?”
“Can we check for hormonal changes?”
“Are there treatments to improve sensitivity or reduce pain?”
Your Pleasure Map 🗺️
Imagine having a personal atlas of your erotic landscape — a living, evolving guide that you can reference and refine over time.
Your map can include:
High-sensitivity zones — external (clitoral glans, labia minora, perineum) and internal (G-spot zone, cervical areas, vestibular bulbs).
Preferred touch styles — light, firm, circular, rhythmic, pulsing.
Contextual factors — environments, moods, and partner dynamics that consistently enhance or diminish arousal.
📌 Pro Tip: Print a simple pelvic diagram or use a secure digital drawing tool. Annotate it with discoveries over time — colors for different sensations, symbols for intensity, and notes for emotional context. Think of it as a pleasure journal in visual form.
Conclusion & What’s Next 🚀
We’ve mapped the visible and hidden landscapes of the body — from the folds of the vulva to the deep wishbone of the clitoral complex, from the pelvic floor’s rhythmic power to the neural highways that light up the brain.
If you take away only one thing from this first installment, let it be this: your orgasm is not a mystery to be solved by luck — it’s an integrated system of nerves, muscles, and blood flow that can be learned, nurtured, and reclaimed.
Coming Up in the Series
Here’s where we’re headed — and where our deep dives will pull back the curtain even further:
Part 2 | Anatomy of an Orgasm
We’ll track what happens from arousal to afterglow — including body cues, brain chemistry shifts, and why timing varies. You’ll also get an Orgasm Mapping Worksheet to begin your own exploration.
Part 3 | “Did I Just Orgasm?”
A reality check for partial orgasms, rolling peaks, and sensations that don’t fit the Hollywood script.
Part 4 | Brain, Hormones & the Big O
A deep dive into neurochemistry, brain regions, and how hormones — from your menstrual cycle to menopause — shape your pleasure.
Part 7 | Barriers to Orgasm (Deep Dive)
From chronic stress to pelvic floor dysfunction, we’ll break down common blocks and show evidence-based solutions.
Part 9 | Impact of Trauma, Birth & Surgery (Deep Dive)
How life events reshape sensation — and how to restore confidence and connection.
Part 12 | The Orgasm Gap & Intersectional Realities
A data-driven look at who’s being left behind and how knowledge, policy, and partner skill can close the gap.
💡 Your Invitation:
Before the next installment, grab a mirror or open an anatomy app. See what’s visible, imagine what’s hidden, and note one question you want answered about your own pleasure. Keep it — we’ll revisit it in our Pleasure Mapping Exercise later in the series.







This is so thorough--THANK YOU! I will be reposting it at 6 AM on Saturday on my Substack page